COVID-19: Update 3 of 3
Who qualifies for COVID-19 screening?
Since COVID symptoms overlap entirely with flu and common cold symptoms, there is no way to tell the difference on exam without performing a test.
For most people, staying at home and isolating from others while you are recoving is recommended. Most common symptoms are fever, cough, headache and muscle aches. It is rare, but sometimes people can develop shortness of breath and chest pain. If this happens, you should seek medical care immediately.
What kind of tests for COVID are available?
There are two types of tests avaialble to determine if you are currently infected with the virus. A third can tell you if you have had, and recovered from the virus.
1- Nasopharengeal Swab: This is a Q-tip that is inserted into your nose and advanced until the tip ends at the back of your nose. It is not a fun test! It makes your eye water and some people sneeze afterwards. This test uses an "RT-PCR" (reverse-transcriptase polymerase chain reaction). The test results can vary based on the sample type and size, the testor's sampling technique, and where in the course of illness you are. False negative rates range from <5% - 40%. Therefore, we don't put a lot of weight in a negative test... we re-test if symptoms are persisting. This is one of the reasons why just getting a test without symptoms is not the best idea for most people. There is no certainty in it.
2- Antibody Blood Test: The is a blood draw that gets sent out to a testing lab to look for antibodies to the coronavirus in your blood, or IgG levels. Antibodies like IgG can take days to weeks to develop, so the validity of your test will depend on when you get the test and how long your body takes to make detectable antibodies.
3- Antigen or "rapid" swab tests: This is the fastest, yet least accurate test. It detects active virus presence in your nose and it quickly performed - like the nasal flu test swabs. A positive test is very accurate, however a negative test is not. [1]
When should I get tested?
In a lot of cases, since testing is not readily avaialble, a diangosis can be made based on symptoms and a recent exposure of someone who is COVID postivie, or who is under invesigation or quarantine themself.
The CDC given recommendations about who should be tested, however the ultimate decision to test rests on the provider and institution that is doing the evaluation. The CDC recommends contacting your healthcare provider or your local health department first.
In general, testing priority is given to those with:
- chronic lung disease, COPD, Asthma
- serious heart conditions; coronary artery disease
- chronic kidney or liver disease; those on hemodialysis
- diabetes
- advanced age; > 65
- morbid or severe obesity; BMI 40 or higher
- immune system compromise; transplant, HIV/AIDS, cancer
and/or to those who:
- are employed in healthcare, or live in a household of a healthcare provider
- are of a marginalized ethnic group
- reside in longterm care facilities, hospitals or prisons
Where can I get tested?
In North Carolina, testing is available at retail pharmacies and WalMart drive throughs, if you qualify. WalMart is providing drive through testing in Elizabethtown, Fayetteville, Greenville, Sylva, Tarboro, Whiteville and Wilkesboro. Certain pharmacies like CVS, Walgreens, Eden Drug and MedicalArts are also testing.
What if I don't qualify for a test?
If you do not qualify for a COVID test, LoginClinics provides a free virtual triage service. Text the words "COVID RAPID SCREEN" to 919-679-1880 and follow the promits. Within minutes you will be connected to a healthcare professional who can evaluate your symptoms, provide recommendations, referrals and even treatment if needed.
LoginClinics uses BlueStream Health's rapid response HIPAA-compliant video conference to meet you, ask questions, and assess your symptoms. During this quick triage it will be determined what your next step should be. If you need treatment, LoginClinics may be able to provide this for you. If you need a doctor excuse note, we will email you one specifiying how long you need to be in isolation and when you can return to work.
What if I have all the symptoms of the coronavirus but no one will test me?
If no one will test you, it generally means that your symptoms are mild or not life threatening and it is believed that you will recover at home in isolation, keeping family members in a separate room and wearing masks when in close proximity. Tylenol can be used for fevers, aches and pains. In addition, there should be frequent hand washing and decontamination of high contact surfaces (door handles, sink knobs, counter tops, etc). If your condition deteriorates, or you develop difficulty breathing, you should seek medical care immediately.
How long do I need to stay in isolation for?
We aren't entirely sure how long one needs to stay in isolation for, however the CDC has some recommendations:
If you had a positive COVID test:
Resolution of fever without the use of fever-reducing medications
AND improvement in respiratory symptoms (eg, cough, shortness of breath)
AND two negative FDA approved COVID-19 tests given at least 24 hours apart.
If you did not get tested, or tested negative and are having symptoms:
At least 10 days have passed since symptoms first appeared
AND at least 72 hours have passed since recovery of symptoms (defined as resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms).
..
..
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
COVID-19: Update 2 of 3
Any particular work enviornments that are at risk of spreading the disease?
Any places of employment that are indoors and have employees in close contact for prolonged periods of time are at risk. Many employers have developed at-work social distancing guidelines, hallway etiquette, the wearing of PPE (personal protective equipment) such as masks and gloves, as well as hand sanitizing guidelines. Grocery stores have arrows on the floors, restaurants and churches are practicing social distancing and most places are recommending the use of a facemask.
What safety controls should be established to limit virus spread?
- Diligent hand washing, particularly after touching surfaces in public OR the use of hand sanitizer that contains at least 60 percent alcohol.
- Practicing good respiratory hygiene- covering your mouth when you cough or sneeze.
- Avoiding touching the face, especially areas of the face where transmission occurs like eyes, nose and mouth.
- Cleaning and disinfecting objects and surfaces that are frequently touched.
- Staying 6 feet apart from other individuals
Who should wear masks?
Masks are recommended when in close contact settings, like work, congregate living, public transportation, etc. - essentially, places where social distancing is difficult. Those under the age of 60 can wear any type of facial mask/covering. One made out of a bandana, t-shirt or fabric. Those 60 years of age or older, or those with medical comorbidities, are recommended to wear a medical mask- as should those who have any type of respiratory infection symptoms if they must leave their home. Remember, wearing a mask doesn’t diminish the importance of continuing to use good respiratory and hand hygiene.
Most places in North Carolina have optional face coverings, but just yesterday Governor Roy Cooper stated the city of Raleigh will require face-coverings in public spaces, along with social distancing. He also vetoed a bill to re-open bars and gyms due to the quickly rising number of cases of COVID and outbreaks in various long term care facilities.
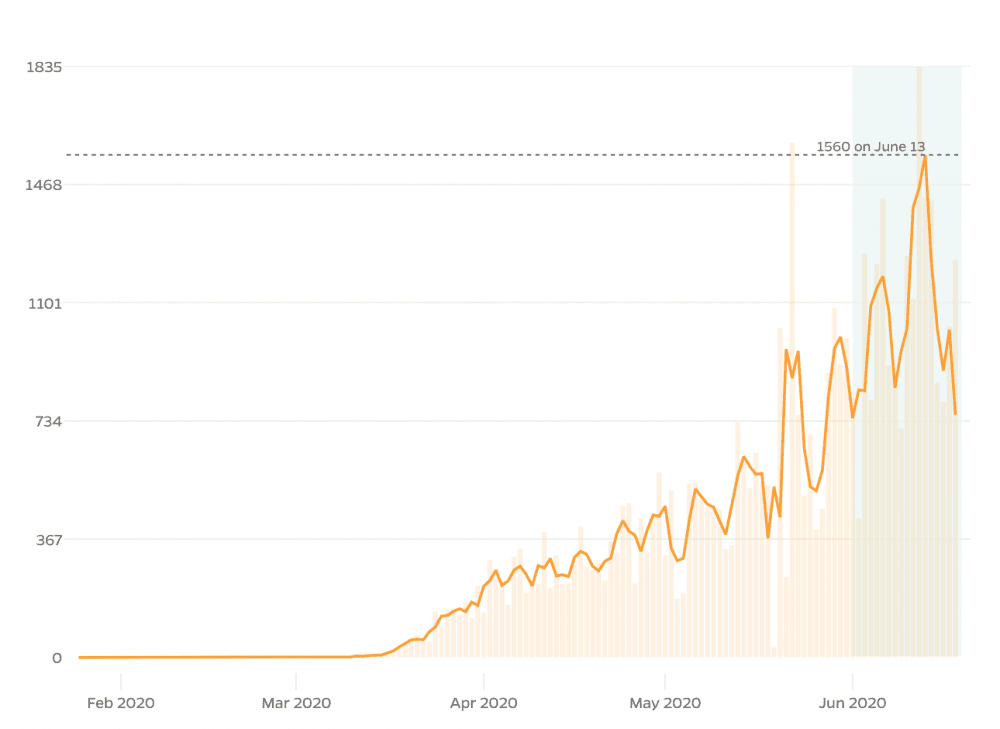
Is NC showing a spike in cases?
In Wake County, we currently have 3,579 confirmed cases, of which, 53% are female and 47% are male, with the city of Raleigh consuming the majority of these cases. [1]
According to the Washington Post COVID tracker, there have been 49,840 reported covid-19 cases state-wide since Feb. 29.

World-wide, there have been a documented 8,687,231 cases, of which the United States has 2,222,576. Of these, 119,131 have died (<1%). [2]
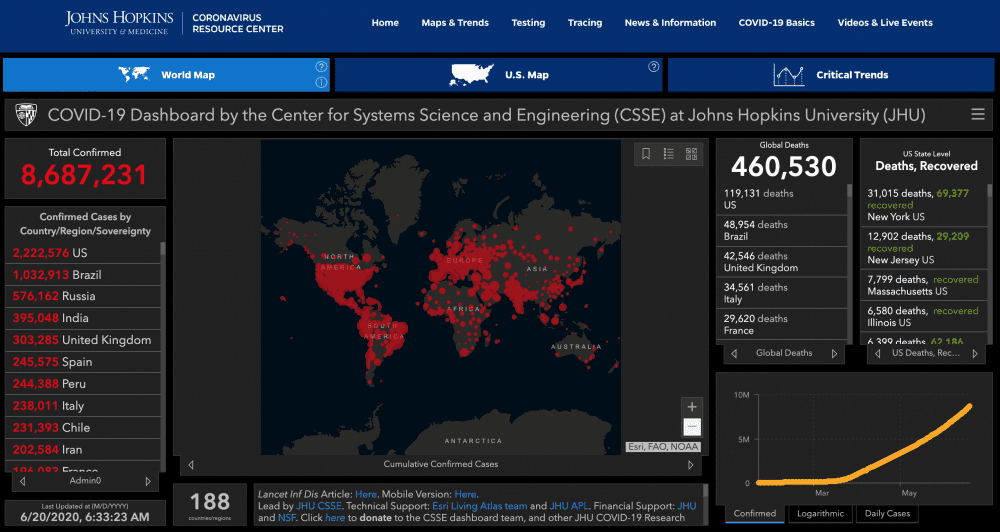
According to this map, North Carolina is currently "flattening the curve" as evidenced by the green background. The number of cases per day, however is rising. [3]
...
Stay tuned for part 3!
- Who qualifies for testing or screening?
- Where should you go to get tested or screened?
- What are antibody tests and when (if ever) should you get one?
- What is a virutal screening and is it effective?
- Who should using virtual screenings?
..
[1] https://covid19.wakegov.com/
[2] https://coronavirus.jhu.edu/map.html
[3] https://coronavirus.jhu.edu/data/new-cases-50-states/north-carolina
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
COVID-19: Update 1 of 3
What is the coronavirus (COVID-19)?
We’ve dealt with the family of coronaviruses for many years as they are responsible for typical common cold symptoms. We previously referred to it as the novel, or new, coronavirus (2019-nCoV). The disease that you contract from the virus is referred to as COVID-19; a disease from the year 2019. Scientists have now re-classified the novel coronavirus as a type of SARS, which stands for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The WHO has identified this as a type of zoonotic infection that has crossed over into the human species. This is referred to as a spillover event and is a known phenomenon. This last happened in 2012 with MERS-CoV, when a spillover came from dromedary camels. So... where did SARS-CoV-2 come from? When virologists look into identifying the source of an infection, they look at it’s genetic makeup. This helps tell virologists what geographic area, or from what species of animal the virus originated. SARS-CoV-2 has been identified to have a similar genetic makeup to viruses that are prevalent in bats and from an area in Asia. This virus in particular is believed to have originated in Wuhan, China.
How long does it take for you to show signs of COVID19 after being exposed?
On average, most people who have contracted the virus will show symptoms 4-5 days after exposure, although there have been some cases documented as early as two days, and as late as 14 days.
What are the common signs and symptoms? [1]
- 50% - Cough
- 43% - Fever (subjective or >100.4°F/38°C) i
- 36 % - Muscle Aches and Pains
- 34% - Headache
- 29% - Shortness of breath
- 20% - Sore throat
- 19% - Diarrhea
- 12% - Nausea and vomitting
- < 10% - loss of smell, taste, abdominal pain and runny nose
Other important statistics:
- 81% have mild or no pneumonia
- 14% have severe disease with shortness of breath, low oxygen levels and more than 50% lung involvement seen on imaginge (CAT scan)
- 5% have critical disease, which includes shock, multi-organ failure and respiratory failure
- 2.3% fatality rate with all deaths having "critical disease"[2]
Can you have the infection and not even know it?
There’s been a lot of talk about what we call “asymptomatic spread”, meaning you have the disease and do not have any symptoms, thereby spreading the virus to others unknowingly. There’s a lot of factors that come into play when considering if and how this is possible. We do know that the virus is detectable for days prior to any symptoms starting, and that is most likely when someone is the most infectious.
This was learned by looking at a break-out in a long term care facility. Many individuals were swab positive and without symptoms for up to six days. Currently, it is believed to be relatively uncommon that this happens and is estimated to be about 6% of those asymptomatically infected are transmitting to others, and maybe about 15% of those who are in close contact, like house-hold members.
Who is at risk of contracting the illness, and from what settings?
Currently most infections come from people who are in close contact with others and for prolonged periods of time, like household contacts, healthcare settings, prisons, cruise ships, nursing homes and long-term care facilities. However, there are documented cases of transmission through non-household contacts like work or social group gatherings. The risk of contracting the virus by passing someone, or handling something they have handled is not well documented and is likely relatively low.
Picking up the virus and becoming infected with it from inanimate objects seems to be a lot lower than originally thought. This is why washing your hands and not touching your face- specifically your mucous membranes in your mouth, eyes and nose are very important. It is believed that this risk is the greatest in households, hospitals, and long-term care facilities where there is a high viral load concentration on objects and surfaces. We know the virus is very susceptible to heat and UV light and only lasts about 15-20 minutes outside and that it can be easily killed in one minutes’ time using appropriate disinfectants. We also know that the amount of time it lives on surfaces depends on the size of the virus particle, the humidity and temperature outside.
...
Stay tuned for parts 2 and 3!
Part 2
- What workplaces are at the highest risk?
- What kind of safety controls should you establish to limit disease exposure and spread?
- Who should wear masks?
Part 3
- Who qualifies for testing or screening?
- Where should you go to get tested or screened?
- What are antibody tests and when (if ever) should you get one?
- What is a virutal screening and is it effective?
- Who should using virtual screenings?
[1] https://www.cdc.gov/mmwr/volumes/69/wr/mm6924e2.htm
[2] https://pubmed.ncbi.nlm.nih.gov/32091533/
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor