Suicide Prevention
September was Suicide Prevention Month and with a suicide taking place approximately every 11 minutes, the month passed and over 3,900 people lost their lives to suicide. While there are many organizations focused on suicide prevention, the most effective prevention work is relational. Here are some practical tips on what to look out for when preventing the suicide of a friend.
WORDS
Listen to the content of your friend’s conversation. According to the National Institute for Mental Health, those who are struggling with suicidal thoughts may talk about wanting to die, great guilt or shame, and being a burden to others. General negative conversation can be normal on occasion, but when that becomes the go-to topic for anyone, this can be cause for concern.
In a world where dark humor is prevalent, the best approach is to have serious conversations with your friends. One way to have this conversation is to ask what’s going on when dark humor is the only kind of jokes they tell. Real conversations are hard, but necessary because suicide is an issue of life and death.
EMOTIONS
Feelings in others are hard to determine, but it is necessary to be on the lookout in order to save a life. Again, the National Institute for Mental Health says feeling empty, hopeless, trapped, extremely sad, more anxious, or even unbearable emotional or physical pain can all be signs of suicidality. There are some signs of these emotions, but the best way is to know how your friends act normally and to be on the lookout for when they are acting out of character.
ACTIONS
The final category of warning signs from the National Institute for Mental Health is a change in behavior. These behaviors include making a plan to die, withdrawing from family and friends, saying goodbye, giving away their possessions, and substance abuse. While these changes can be obvious, one must know how their friend acts on a day-to-day basis in order to recognize the change.
WHAT NOW?
The easiest way to check on your friend is to simply ask, “Are you okay?” and be prepared to genuinely listen. This shows your friend that you care about them and that you have noticed their recent actions. Many suicides are what some have called “deaths of despair” meaning they feel hopeless and alone. Reaching out to them shows them they are not alone and that there is someone they can talk to.
What happens when they share things you are not prepared to hear? Do not overreact. This can lead them to feel guilty and as if they are a burden. Encourage them to seek professional help. Even offering to go with them to a counselor can show them the support they need.
If you or someone you know is struggling with suicidal thoughts, the National Suicide Helpline now has a three-digit crisis line that can receive calls or texts. That number is 988.
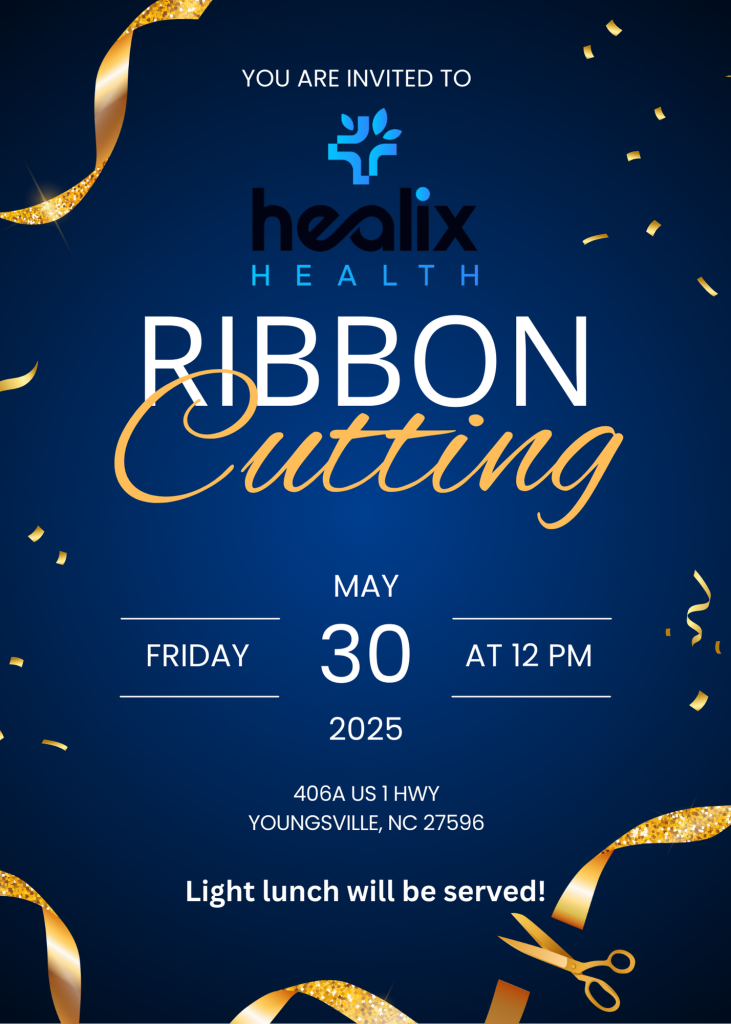
Public Invited to LoginClinics Open House March 31
LoginClinics, a telemedicine health services clinic, is inviting the public and patients to visit its new brick-and-mortar location during an open house “homecoming” on Thursday, March 31, 2022, 4 p.m. – 6 p.m. The new address is 406-A US Hwy 1, Youngsville, NC 27596.
Nurse Practitioner and Founder Jaclyn Qualter is calling the free event a “homecoming” with the opportunity for guests to learn more about services while enjoying refreshments and meeting the staff.

“This open house is more of a homecoming to welcome the community along with our new and existing clients and patients to learn about our health and employee services and see our new facility. We began offering telehealth in 2019 and want to share this new chapter in our growth,” Qualter explained.
The new clinic, formerly in a space occupied by an insurance agency, is 1300 square feet with a reception area, self-check-in bar, exam room, medical testing lab and a large multi-purpose room for employee training and testing.
In addition to telemedicine, LoginClinics services include patient exams, lab work, employee, CDL and firefighter physicals, urine drug screens, CPR training and COVID testing and treatment. The new facility will accommodate patients and employers in the northeastern counties of the Triangle including Wake, Franklin, Granville and beyond.
LoginClinics Opens New Health Clinic in Youngsville
Office Visits and Employer Health Services Now an Option along with Telehealth
(Youngsville, N.C., February 8 , 2022) – LoginClinics, building on its foundation of telemedicine health services, announces the opening of a new brick-and-mortar location in Youngsville, N.C., in March 2022.
Founded in 2019 as one of the first telemed mobile providers in the Wake Forest-Youngsville area by Nurse Practitioner Jaclyn Qualter, LoginClinics has grown from offering patients online medical care from their smartphones or internet-connected webcams to in-person exams and lab work as well as employee health and safety services.
Located at 406-A US Hwy 1, Youngsville, NC 27596, the new facility will accommodate patients and employers in the northeastern counties of the Triangle including Wake, Franklin, Granville and beyond. In addition to telemedicine, services will include patient exams, lab work, employee, CDL and firefighter physicals, urine drug screens, CPR training and COVID testing and treatment.
The new space, formerly an insurance agency, is 1300 square feet with a reception area, self-check-in bar, exam room, medical testing lab and a large multi-purpose room for employee training and testing.
LoginClinics new location addresses an unmet need in healthcare delivery by filling the gap between telemedicine and facility-based services previously only met by urgent care or large hospitals.
“LoginClinics has streamlined and personalized the telehealth process and now patients can be seen in our new local clinic, when necessary,” explained Qualter. “We’ve learned sometimes telemed is not enough and the patient needs an in-person exam or lab work.” She added that they are not an urgent care facility.
Currently employing five health professionals, Qualter says the LoginClinics staff will grow to seven. Hours of the new location will be Monday through Friday, 8:30 a.m. - 5 pm. Weekend hours are by appointment via texting 919-679-1880. The on-call staff will respond within an hour.
LoginClinics is inviting the public and patients to visit the new health clinic during an open house on Thursday, March 31, 2022, 4 p.m. – 6 p.m. Qualter is calling the event a “homecoming” with the opportunity to learn more about services being offered while enjoying refreshments and meeting the staff.
To schedule an appointment or learn more visit www.healixhealthclinics.com or call 919-679-1880.
About LoginClinics
LoginClinics, PLLC, offers patients telemedicine services through smart phones or internet-connected webcams, and now a local health clinic at 406-A US Hwy 1, Youngsville, North Carolina. Founded in 2019 by Jaclyn Qualter, a nurse practitioner and health care mentor, LoginClinics offers patient exams and lab work as well as employee health and safety services. More information can be found online at www.LoginClinics.com,www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
COVID-19: Update 3 of 3
Who qualifies for COVID-19 screening?
Since COVID symptoms overlap entirely with flu and common cold symptoms, there is no way to tell the difference on exam without performing a test.
For most people, staying at home and isolating from others while you are recoving is recommended. Most common symptoms are fever, cough, headache and muscle aches. It is rare, but sometimes people can develop shortness of breath and chest pain. If this happens, you should seek medical care immediately.
What kind of tests for COVID are available?
There are two types of tests avaialble to determine if you are currently infected with the virus. A third can tell you if you have had, and recovered from the virus.
1- Nasopharengeal Swab: This is a Q-tip that is inserted into your nose and advanced until the tip ends at the back of your nose. It is not a fun test! It makes your eye water and some people sneeze afterwards. This test uses an "RT-PCR" (reverse-transcriptase polymerase chain reaction). The test results can vary based on the sample type and size, the testor's sampling technique, and where in the course of illness you are. False negative rates range from <5% - 40%. Therefore, we don't put a lot of weight in a negative test... we re-test if symptoms are persisting. This is one of the reasons why just getting a test without symptoms is not the best idea for most people. There is no certainty in it.
2- Antibody Blood Test: The is a blood draw that gets sent out to a testing lab to look for antibodies to the coronavirus in your blood, or IgG levels. Antibodies like IgG can take days to weeks to develop, so the validity of your test will depend on when you get the test and how long your body takes to make detectable antibodies.
3- Antigen or "rapid" swab tests: This is the fastest, yet least accurate test. It detects active virus presence in your nose and it quickly performed - like the nasal flu test swabs. A positive test is very accurate, however a negative test is not. [1]
When should I get tested?
In a lot of cases, since testing is not readily avaialble, a diangosis can be made based on symptoms and a recent exposure of someone who is COVID postivie, or who is under invesigation or quarantine themself.
The CDC given recommendations about who should be tested, however the ultimate decision to test rests on the provider and institution that is doing the evaluation. The CDC recommends contacting your healthcare provider or your local health department first.
In general, testing priority is given to those with:
- chronic lung disease, COPD, Asthma
- serious heart conditions; coronary artery disease
- chronic kidney or liver disease; those on hemodialysis
- diabetes
- advanced age; > 65
- morbid or severe obesity; BMI 40 or higher
- immune system compromise; transplant, HIV/AIDS, cancer
and/or to those who:
- are employed in healthcare, or live in a household of a healthcare provider
- are of a marginalized ethnic group
- reside in longterm care facilities, hospitals or prisons
Where can I get tested?
In North Carolina, testing is available at retail pharmacies and WalMart drive throughs, if you qualify. WalMart is providing drive through testing in Elizabethtown, Fayetteville, Greenville, Sylva, Tarboro, Whiteville and Wilkesboro. Certain pharmacies like CVS, Walgreens, Eden Drug and MedicalArts are also testing.
What if I don't qualify for a test?
If you do not qualify for a COVID test, LoginClinics provides a free virtual triage service. Text the words "COVID RAPID SCREEN" to 919-679-1880 and follow the promits. Within minutes you will be connected to a healthcare professional who can evaluate your symptoms, provide recommendations, referrals and even treatment if needed.
LoginClinics uses BlueStream Health's rapid response HIPAA-compliant video conference to meet you, ask questions, and assess your symptoms. During this quick triage it will be determined what your next step should be. If you need treatment, LoginClinics may be able to provide this for you. If you need a doctor excuse note, we will email you one specifiying how long you need to be in isolation and when you can return to work.
What if I have all the symptoms of the coronavirus but no one will test me?
If no one will test you, it generally means that your symptoms are mild or not life threatening and it is believed that you will recover at home in isolation, keeping family members in a separate room and wearing masks when in close proximity. Tylenol can be used for fevers, aches and pains. In addition, there should be frequent hand washing and decontamination of high contact surfaces (door handles, sink knobs, counter tops, etc). If your condition deteriorates, or you develop difficulty breathing, you should seek medical care immediately.
How long do I need to stay in isolation for?
We aren't entirely sure how long one needs to stay in isolation for, however the CDC has some recommendations:
If you had a positive COVID test:
Resolution of fever without the use of fever-reducing medications
AND improvement in respiratory symptoms (eg, cough, shortness of breath)
AND two negative FDA approved COVID-19 tests given at least 24 hours apart.
If you did not get tested, or tested negative and are having symptoms:
At least 10 days have passed since symptoms first appeared
AND at least 72 hours have passed since recovery of symptoms (defined as resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms).
..
..
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
COVID-19: Update 2 of 3
Any particular work enviornments that are at risk of spreading the disease?
Any places of employment that are indoors and have employees in close contact for prolonged periods of time are at risk. Many employers have developed at-work social distancing guidelines, hallway etiquette, the wearing of PPE (personal protective equipment) such as masks and gloves, as well as hand sanitizing guidelines. Grocery stores have arrows on the floors, restaurants and churches are practicing social distancing and most places are recommending the use of a facemask.
What safety controls should be established to limit virus spread?
- Diligent hand washing, particularly after touching surfaces in public OR the use of hand sanitizer that contains at least 60 percent alcohol.
- Practicing good respiratory hygiene- covering your mouth when you cough or sneeze.
- Avoiding touching the face, especially areas of the face where transmission occurs like eyes, nose and mouth.
- Cleaning and disinfecting objects and surfaces that are frequently touched.
- Staying 6 feet apart from other individuals
Who should wear masks?
Masks are recommended when in close contact settings, like work, congregate living, public transportation, etc. - essentially, places where social distancing is difficult. Those under the age of 60 can wear any type of facial mask/covering. One made out of a bandana, t-shirt or fabric. Those 60 years of age or older, or those with medical comorbidities, are recommended to wear a medical mask- as should those who have any type of respiratory infection symptoms if they must leave their home. Remember, wearing a mask doesn’t diminish the importance of continuing to use good respiratory and hand hygiene.
Most places in North Carolina have optional face coverings, but just yesterday Governor Roy Cooper stated the city of Raleigh will require face-coverings in public spaces, along with social distancing. He also vetoed a bill to re-open bars and gyms due to the quickly rising number of cases of COVID and outbreaks in various long term care facilities.
Is NC showing a spike in cases?
In Wake County, we currently have 3,579 confirmed cases, of which, 53% are female and 47% are male, with the city of Raleigh consuming the majority of these cases. [1]
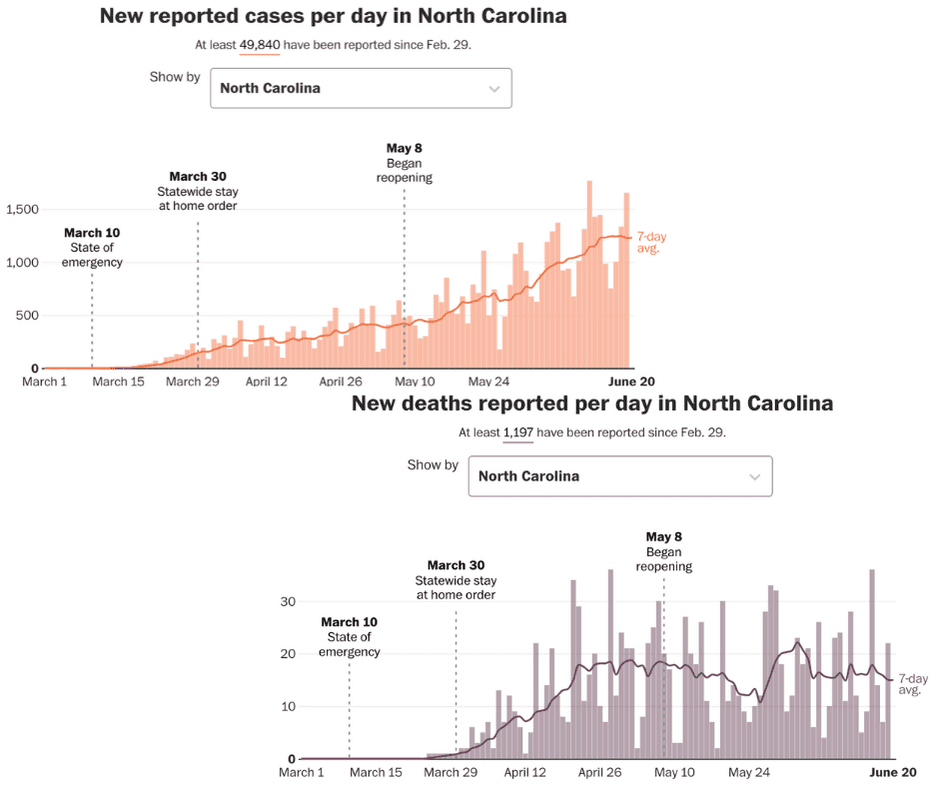
According to the Washington Post COVID tracker, there have been 49,840 reported covid-19 cases state-wide since Feb. 29.
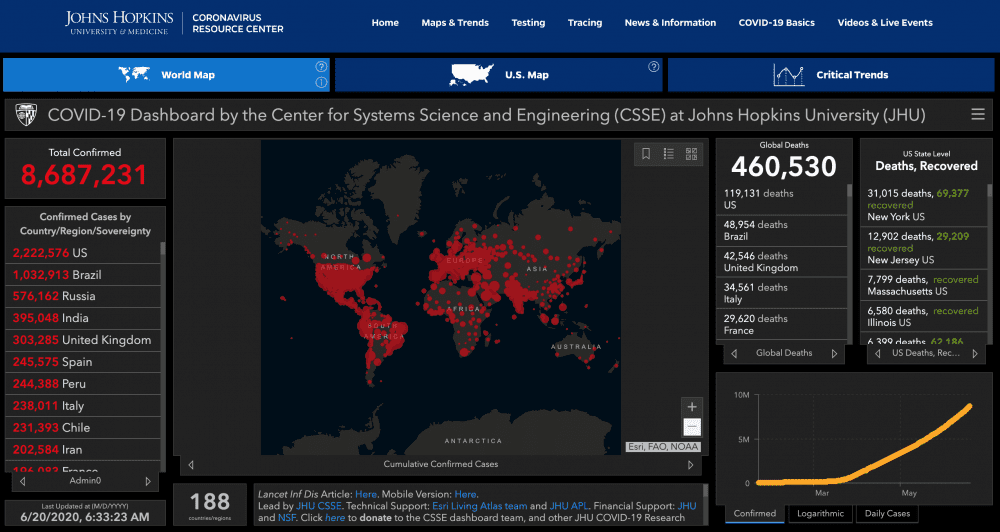
World-wide, there have been a documented 8,687,231 cases, of which the United States has 2,222,576. Of these, 119,131 have died (<1%). [2]
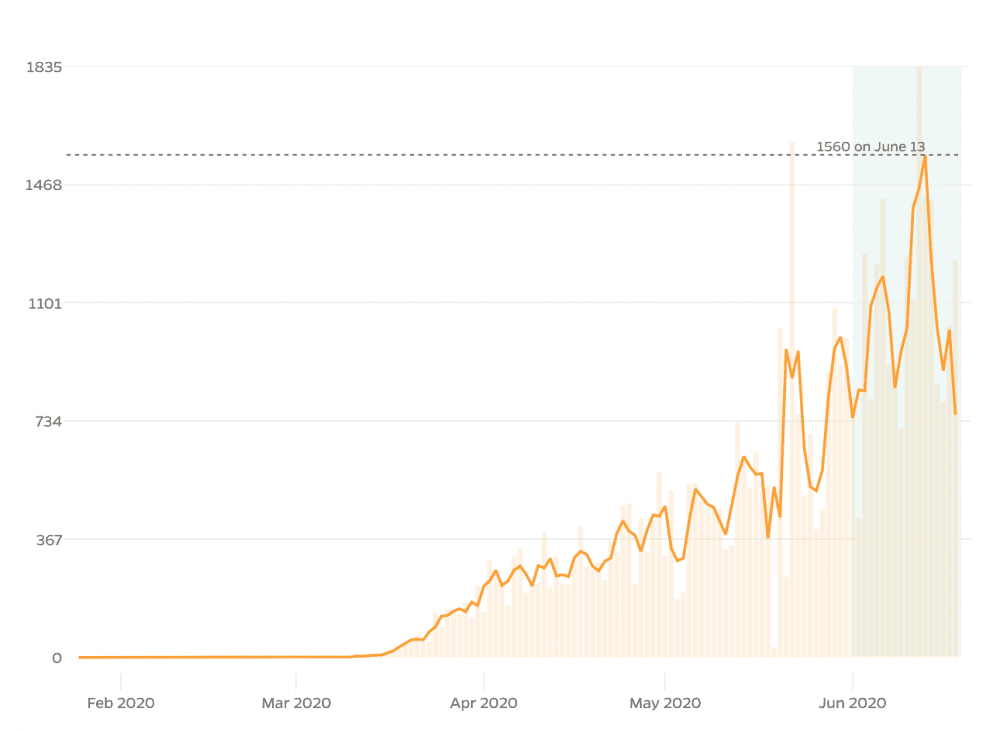
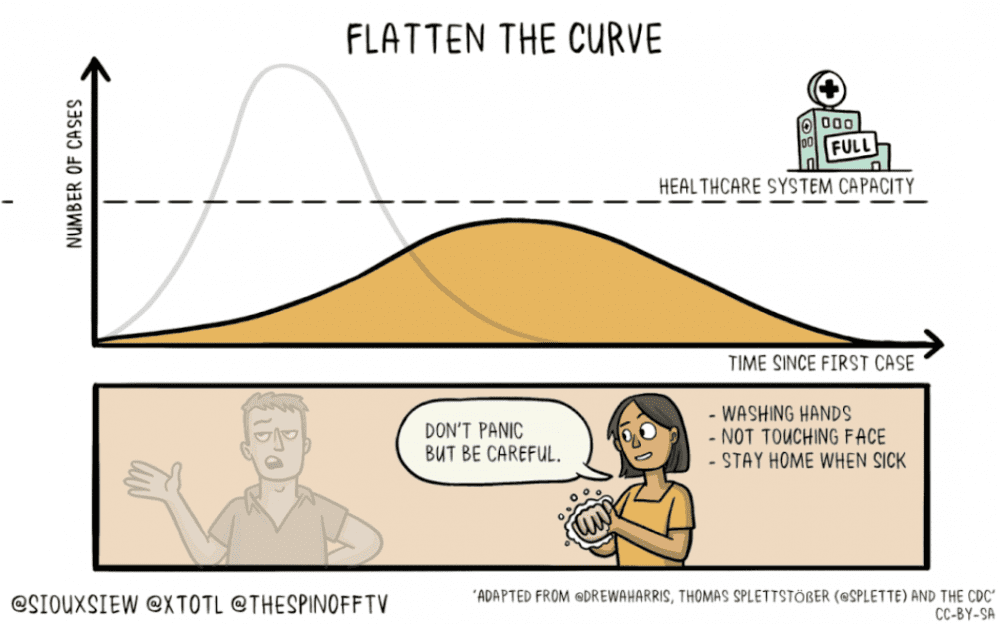
According to this map, North Carolina is currently "flattening the curve" as evidenced by the green background. The number of cases per day, however is rising. [3]
...
Stay tuned for part 3!
- Who qualifies for testing or screening?
- Where should you go to get tested or screened?
- What are antibody tests and when (if ever) should you get one?
- What is a virutal screening and is it effective?
- Who should using virtual screenings?
..
[1] https://covid19.wakegov.com/
[2] https://coronavirus.jhu.edu/map.html
[3] https://coronavirus.jhu.edu/data/new-cases-50-states/north-carolina
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
COVID-19: Update 1 of 3
What is the coronavirus (COVID-19)?
We’ve dealt with the family of coronaviruses for many years as they are responsible for typical common cold symptoms. We previously referred to it as the novel, or new, coronavirus (2019-nCoV). The disease that you contract from the virus is referred to as COVID-19; a disease from the year 2019. Scientists have now re-classified the novel coronavirus as a type of SARS, which stands for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The WHO has identified this as a type of zoonotic infection that has crossed over into the human species. This is referred to as a spillover event and is a known phenomenon. This last happened in 2012 with MERS-CoV, when a spillover came from dromedary camels. So... where did SARS-CoV-2 come from? When virologists look into identifying the source of an infection, they look at it’s genetic makeup. This helps tell virologists what geographic area, or from what species of animal the virus originated. SARS-CoV-2 has been identified to have a similar genetic makeup to viruses that are prevalent in bats and from an area in Asia. This virus in particular is believed to have originated in Wuhan, China.
How long does it take for you to show signs of COVID19 after being exposed?
On average, most people who have contracted the virus will show symptoms 4-5 days after exposure, although there have been some cases documented as early as two days, and as late as 14 days.
What are the common signs and symptoms? [1]
- 50% - Cough
- 43% - Fever (subjective or >100.4°F/38°C) i
- 36 % - Muscle Aches and Pains
- 34% - Headache
- 29% - Shortness of breath
- 20% - Sore throat
- 19% - Diarrhea
- 12% - Nausea and vomitting
- < 10% - loss of smell, taste, abdominal pain and runny nose
Other important statistics:
- 81% have mild or no pneumonia
- 14% have severe disease with shortness of breath, low oxygen levels and more than 50% lung involvement seen on imaginge (CAT scan)
- 5% have critical disease, which includes shock, multi-organ failure and respiratory failure
- 2.3% fatality rate with all deaths having "critical disease"[2]
Can you have the infection and not even know it?
There’s been a lot of talk about what we call “asymptomatic spread”, meaning you have the disease and do not have any symptoms, thereby spreading the virus to others unknowingly. There’s a lot of factors that come into play when considering if and how this is possible. We do know that the virus is detectable for days prior to any symptoms starting, and that is most likely when someone is the most infectious.
This was learned by looking at a break-out in a long term care facility. Many individuals were swab positive and without symptoms for up to six days. Currently, it is believed to be relatively uncommon that this happens and is estimated to be about 6% of those asymptomatically infected are transmitting to others, and maybe about 15% of those who are in close contact, like house-hold members.
Who is at risk of contracting the illness, and from what settings?
Currently most infections come from people who are in close contact with others and for prolonged periods of time, like household contacts, healthcare settings, prisons, cruise ships, nursing homes and long-term care facilities. However, there are documented cases of transmission through non-household contacts like work or social group gatherings. The risk of contracting the virus by passing someone, or handling something they have handled is not well documented and is likely relatively low.
Picking up the virus and becoming infected with it from inanimate objects seems to be a lot lower than originally thought. This is why washing your hands and not touching your face- specifically your mucous membranes in your mouth, eyes and nose are very important. It is believed that this risk is the greatest in households, hospitals, and long-term care facilities where there is a high viral load concentration on objects and surfaces. We know the virus is very susceptible to heat and UV light and only lasts about 15-20 minutes outside and that it can be easily killed in one minutes’ time using appropriate disinfectants. We also know that the amount of time it lives on surfaces depends on the size of the virus particle, the humidity and temperature outside.
...
Stay tuned for parts 2 and 3!
Part 2
- What workplaces are at the highest risk?
- What kind of safety controls should you establish to limit disease exposure and spread?
- Who should wear masks?
Part 3
- Who qualifies for testing or screening?
- Where should you go to get tested or screened?
- What are antibody tests and when (if ever) should you get one?
- What is a virutal screening and is it effective?
- Who should using virtual screenings?
[1] https://www.cdc.gov/mmwr/volumes/69/wr/mm6924e2.htm
[2] https://pubmed.ncbi.nlm.nih.gov/32091533/
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
The Truth About Masks
I’ve been wearing a mask for the past two weeks anytime I have to go to the grocery store. It’s an odd feeling for me to walk around and be the only person in the store wearing one. As a Nurse Practitioner, I know that a mask will protect me and others so I’m confused when I get disgusted glares and eye rolls. Interestingly, I see many people with gloves on- and that’s well received- but no masks. So what’s the truth about masks and why is there so much social shame over wearing one?
Last week my daughter and I went into the store with our masks on and met a shopper who was clearly disturbed by us. As we passed in the aisle she said to her husband, “This is absurd!! These people are nuts!” My daughter asked me if I heard what the woman said about us- it was a great teaching moment for me. I was able to explain to her that this will be a common situation she will encounter in life and that she needs to understand her convictions and not be swayed by the opinions- or disgust- of others. I also explained to her that this woman clearly was suffering from some form of anxiety or denial that our mere presence with masks on gave her such a visceral reaction. It was a way for me to show empathy for this woman instead of anger; to promote a more peaceful and loving way of living for my daughter.
As we were leaving the store we saw an elderly woman wearing a mask. I greeted her with a light-hearted, “Hello, my masked friend!”. She turned around ready to defend herself, but when she saw both of us in our masks her countenance relaxed and her eyes smiled. She said “You know, I’ve suffered a lot by wearing this mask out in public, but I don’t care. I’m 67 and my immune system isn’t what it used to be.” I lovingly affirmed her and told her if others wanted to shame or bully her, there was something incredibly wrong with them. After wishing her well, I turned around and right behind me was the angry woman we saw earlier, frozen and speechless. I am hopeful she heard our full exchange and in the future would choose to share compassion instead of anger.
There are many expensive and complex “respirators” available for purchase and use and two primary disposable face masks, the N95 and a surgical mask. The N95 is tight fitting and reduces exposure to large droplets, small particles and small particle aerosols. A surgical mask is loose fitting and protects the wearer against large droplets, splashes and sprays.
Surgical
Surgical masks are made to fit loosely over your mouth and nose with elastic loops that wrap around your ears and a pliable metal strip to form along the nasal bridge. This mask does not completely filter all of the air you breathe in and out because it is loose on each side and allows air to "leak". It does however, protect those around you from your respiratory droplets.
In the hospital, we wear these masks if we are sick so we do not infect other healthcare workers or patients, but we also wear them during a surgical or sterile procedure to protect the sterile field.
Wearing a mask like this in public will most certainly provide more protection than not wearing a mask at all. Primarily you will be protecting others from yourself. If everyone wears a mask when they go to the grocery or any other essential store, the chances of becoming infected or spreading infection will dramatically decrease. If you do not have a surgical mask, there are a variety of free patterns available online for use. If you’re not the Joann Fabrics type, the Surgeon General made this video which shows how to quickly make a nice mask!
N95
There are different sizes of these masks; small, medium and large. "N" means "not resistant to oil". When worn properly, these masks provide 95+% air filtration and eliminates small particles- like those from the coronavirus- from being inhaled. You must have a clean face to wear this mask properly (no beards or makeup). The coronavirus is 0.6 microns in size and can travel through other fabrics like cotton or surgical masks. Conversely, when not assessed for proper fit, the mask can "leak" and is ineffective.
Unfortunately, not everyone can wear these masks. This type of respirator can make breathing more difficult because of the carbon dioxide buildup inside of the mask, which in turn reduces the amount of oxygen inhaled and subsequent oxygen exchange thereby increasing your respiratory and heart rate. If you have one of the following health conditions, please check with your nurse practitioner or doctor before you decide to purchase and wear an N95:
- Chronic Obstructive Pulmonary Disease (COPD)
- Morbid Obesity (Body Mass Index > 40)
- Chronic Heart Disease
- Chronic Lung Disease
- Claustrophobia
- Panic Attacks
New Recommendations by CDC and Trump Administration
President Trump announced new guidance this past Friday for people in the United States to wear some type of face covering when out in public. This recommendation is made in an effort to slow the spread of the coronavirus, which as you may recall was a reversal from their recommendations prior to last week.
The CDC “recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.” If you’re not sure how to properly wear a mask, the CDC has a fantastic website with most of what you need to know, like how to properly wear one, when to wash it, how to make one, what materials to use, and so on. If you’re a low maintenance/no fluff type of guy or gal, the US Surgeon General, Jerome Adams shows how to make a mask in 20 seconds out of common household items.
What Does the Scientific Data Say?
In order for us to know what type of mask may work, we need to know more about the coronavirus; it’s size and how it’s transmitted. Since the coronavirus is still so new to us, we truly don’t know exactly how protective different masks are against this virus. We can however, guess based on what we know from other masks and other viruses, but ultimately only with time and experience will we find the truth.
How is the Coronavirus Transmitted?
- Respiratory Droplet: This is theorized to be the primary way the virus is spread. Droplets are large and heavy. They are released by an infected person when this person coughs, sneezes, talks or breathes. In a ballistic fashion they fly out about 6.5 feet before falling to the ground. Surgical masks, face clothes or a bandana around your nose and mouth area, would work to protect you against droplet transmission of the virus.
- Respiratory Aerosolization: This route of transmission is thought to be a secondary way of transmitting the virus and a big concern for healthcare workers. These particles of the virus are very tiny and can stay suspended in the air for minutes to hours. An N95 mask is needed to protect at-risk healthcare workers from contracting the virus from their infected patients, especially when intubating, suctioning or bagging an infected patient.
- Direct Contact: Virus particles can rest on an inanimate surface and also be transferred by human hands, thus being moved from one place or person to another. Depending on the type of surface the virus lands on, it can stay viable and infectious anywhere from four hours to three days. It is theorized that the cornavirus behaves in the same manner as other SARS viruses so it is still very very important to wash your hands and not touch your face even if you are wearing a mask. You need to wash your hands before AND after you put your facemask on and off.
Do Masks Work?
In a recent commentary in The Lancet, a group of UK and Hong Kong researchers looked at the existing scientific evidence for wearing a mask as well as the efficacy. They researchers recognize lack of supportive data for ubiquitous mask use but also note the inconsistencies in recommendations around the globe. They conclude that even though data is lacking, it is reasonable for those who are high risk, as well as those who are having symptoms to wear a mask when out in public. They also postulate that there is evidence of novel coronavirusa “community spread”, meaning the infection is being spread before people develop symptoms. Therefore, if an asymptomatic and unknowingly positive person wears a mask, he or she will be protecting others around them. They conclude with reminding us that wearing a mask is not a substitute for good hand hygiene and social distancing. It is “just one more layer of protection”.
What we absolutely do know is that the virus appears to not be as aggressive as measles which carries a 30% mortality and is highly infectious. For every one person with measles, that one person infects about another 12-13 persons.
Not so with COVID19: For every one person with the novel coronavirus, 2-3 other persons are infected. This has led scientists to assume that the virus is spread primarily through droplets and a surgical mask would probably be effective in reducing the risk or spread.
To back this up with some data, I read two studies that looked at penetration rates for different particles sizes based on the type of mask. (NIOSH, 2010 and Air Quality Reseachers, 2014). The results were widely discrepant and are on average, as follows:
- N95 > 90%
- Dental mask 60%
- Surgical Masks 40%
- Towel Masks 40%
- Sweatshirt Masks, 20-40%
- Scarf Masks 20%
- Shirt Masks 10%
- Handmade Cotton Masks 2% (one layer)-13% (four layers)
The authors did note that a lot of these masks did not control for "leakage" and that was identified as possibly one of the largest problems. They recommended using pantyhose to help the mask adhere to your face (Think Spanx) and in doing so, they noted you could decrease leakage to < 10% for homemade masks and < 1% for surgical masks.
So What Should You Do?
If you are healthy, you must continue to prioritize and fully participate in social distancing measures as this is the only 100% tried and true protection against transmission. You must also continue to avoid touching your face and wash your hands often; especially after you sneeze, cough or blow your nose. Of course, if you need to go out to the grocery store, you should continue to use social distancing measures plus choose some sort of facial covering when you are out. I know there’s a mad rush for surgical masks but considering the above data, a towel mask would work just a well - and also may be easier to get. Consider using a hand towel the way the US Attorney General did with a Tshirt and adding some Spanx on top of any other mask to prevent leakage. The study found that leakage was reduced to < 10% around a handkerchief and < 1% around a surgical mask.
If you develop any type of respiratory symptoms such as sore throat, runny nose, fevers or cough, please isolate yourself away from your immediate family- as well as others- and notify your nurse practitioner or doctor. If you do not have a nurse practitioner or doctor, you can use a TeleMedicine platform like LoginClinics. LoginClinics is currently providing free rapid virtual screenings for the coronavirus in an effort to educate and connect people to local resources, if indicated.
Finally, be loving and accepting towards others who decide to wear (or not wear) a mask out in public. Continue to maintain social distancing standards until instructed otherwise. Expect expert opinions to change with the tides of this illness. Something recommended yesterday may not be recommended tomorrow. Be patient - we are all learning together. Extend neighborly kindness to those you happen to encounter when you are out (and in on Zoom calls) as you do not know what trials and challenges they are facing today. Recognize that we are all in this together, as a nation and people. This too shall pass… doesn’t matter what type of mask we use (or don’t use).
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
Blended Family Challenges During the COVID19 Pandemic
Two weekends ago when everyone was heeding advice from local and federal authorities to stay home- including myself and my husband- my stepdaughter went to a convention in Asheville. Because of our concerns about COVID exposure, my husband reached out to his ex about the trip. He was told she felt safe taking her and discussed with his daughter they would not hug anyone while they were there. The week following the convention my husband was on the phone with his kids and his daughter volunteered that Mom “has fevers and body aches”. Of course we were concerned so my husband reached out again to his ex-wife via email and she responded days later with a less than reassuring response.
This comes in stark contrast to the message I received from my ex. He has been texting me for weeks now with article links about COVID and is on Fort Knox isolated lockdown, complete with an insta-greenhouse and food delivery trucks. He believes my occupation places him and his step kids at risk and he has asked for our kids to stay with him until COVID is eradicated.
As you can imagine, step and co-parenting can be challenging, especially if communications from the other households are sparse, and beliefs about what is best for each household are conflicting. As a stepmom of almost eight years, I’m used to not being able to control what happens in the other parents’ homes. I’m also used to unintentionally sharing socks, lunchboxes, attitudes and the flu. I am fully aware that each decision made by one household can potentially affect the other three.
Especially now, both parents and families need to be on the same page. They need to discuss the plans for custody right now, but also need to have a plan in place if someone becomes ill. I talked to LoginClinics’ Therapist Sarah Harris, LMFT about my dilemma this weekend. She offered some steps to take when considering custodial time changes during the COVID pandemic.
Remove your emotions and stick to the facts.
Calm yourself and find a way to stay grounded amidst all of the chaos and uncertainty that is going on. If you get caught up in just the emotional component of things, you lose clarity of thought and end up choosing unhealthy responses and plans that do not put the children first. If you do not know how to stay grounded, or need help with mindfulness-based stress reduction, call us ;)
Stay rational about the situation.
Make sure you are making the kids your utmost priority. Use clear and open communication with each other about the situation and your concerns with the children. This is not about you, this is about what’s best for your kids. You need to love your kids more than you love yourself.
Put all of the possible options out on the table.
Let the other parent know which one of these options you are comfortable with, and which you are not. It’s also important to be realistic and practical when considering what these options are. You cannot control every possible risk, so be mindful to not go to extremes when offering solutions.
Pick the resolution that both of you agree on.
Out of all of the possible (rational) options, there is bound to be a middle ground that the both of you can agree on. If you have concerns about the other partner- what they might be doing- keep these discussions away from the children. The last thing our kids need is our anxiety projected on them and making them feel like they need to choose sides.
From a medical perspective you also need to consider what will be done if anyone in either household becomes ill. Currently Wake County is under Governor Cooper’s “Stay at Home” order so presumably there should not be much in the way of exposure, but given the odd carrier status and long incubation of this virus you just never know. You may think it’s safe to have a drink on your back porch with your neighbor or go to the grocery store without a mask, but it may not be. None of us have a crystal ball. Here are some ways that you can protect yourself and your family as well as providing reassurance for your children:
Make a plan and put it in writing.
If you don’t have participation or agreement from the other household, that’s okay. You can still actively communicate your status and symptoms to them even if they don’t respond. In your plan, specifically mention what you will do if you or your children develop any upper respiratory infection symptoms. A good way to instill trust and show you are keeping communication channels open is to report your status to the other household on the exchange day via text or email. This will be easy for me because I always give a “report” to my kids’ Father on exchange day but now I also include health status updates. Here’s a text I sent before they tracked out:
“VV and I studied tonight for her science test friday- quiz code is 3441420 she still is getting a 70%. Also, David has decided he wants to practice driving so we have been doing that as well. He’s actually pretty good and even drove to school this morning. He’s a little unclear as to who has the right of way when it comes to intersections and turning. Additionally, I just purchased some Airborne gummies and Elderberry gummies to help keep their immune systems strong.”
Implement health-boosting measures.
Sleep: I’m always on a health tirade with my kids, but now even more so. They are out of school and thrive with more structure and routine (as does my sanity). Both structure and routine help the body and the brain to operate optimally. Even though we are tracked out my kids still have a routine bedtime. It’s two hours later than when they are in school and they also get to sleep in an extra two hours. Wake up times are consistent however, so no one sleeps past 10 or 11 am.
Supplements: My kids are taking Elderberry, Vitamin C and Airborne supplements daily, along with a multivitamin. I generally am not a promoter of vitamins if one eats a healthy diet and has no nutritional deficiencies, however we know that these immune systems boosters do just that.
Exercise: Scientific studies has proven over and over that moderate exercise most days of the week actually boosts and strengthens your immune system. It improves immune system regulation as well as delaying the onset of age-related dysfunction. Exercise also stimulates various pathways in the body to promote a decrease in inflammation. I’ve recently found the practice of Yoga and find it to be perfect for a mind and body workout.
Brain Games and Reading : We know that mental and physical health go hand-in-hand. If your brain is filled with anxious or depressing thoughts, your body and immune system can be weakened. Taking time to focus on a good book or playing cards or board games with family members you love can release those healthy brain neurotransmitters and keep your immune system strong.
This is an unprecedented time for the majority of us with the threat of anxiety and depression lurking around every corner. In my four decades of life I have never seen anything like this. I have anecdotally heard about the devastation caused by polio, smallpox and measles but have not experienced it first-hand. I was born after these diseases were eradicated.
I’ve been a nurse for twenty-two years and a nurse practitioner for fifteen. I’ve taken care of tuberculosis patients on respiratory isolation and patients in cholera camps in Haiti. I’ve been stuck by needles used on patients and have witnessed some really scary medical situations in both the trauma center and ICUs I have worked in. I am trained in sterile procedures and how to maintain said sterility. I worked in interventional radiology for a decade placing chest ports for chemotherapy utilizing the utmost of sterile conditions. I know how to put on and take off PPE (personal protective equipment) with the best of them. I am not a fearful person and I do not live in a state of fear. During this time I continue to live my life and enjoy the time with my kids and husband making the most out of the days that I have- life is short and not guaranteed.
The last thing any of us need right now is more added stress and speculation about things that may never come to pass. The best we can do is put our children first. Communicate openly and honestly with our co-parent. Stay focused on the good. Promote physical and mental health and wellness in your immediate household. Do not focus on the activities (or lack thereof) in the other household your kids live in. Practice good eating and sleep practices. Exercise. Meditate. Do Yoga. PRAY.
Extend love and kindness to your immediate family and to those outside it.
Parenting Time Considerations During the COVID19 Pandemic
Child Custody Arrangements Amid Coronavirus: Statewide Family Law Panel Issues Guidance
7 Guidelines for Parents Sharing Custody of Children During the COVID19 Pandemic
Coronavirus: Children Can Visit Separated Parents During Restrictions
Quarantines and Custody Agreements: How do Divorced Parents Handle the Coronavirus?
COVIDs Impact on Child Custody and Divorce in Colorado
How to Help Kids Sort Fact from Fiction About the Coronavirus
Planning Ahead Helps Make Blended Families Work
Helping Children Cope with Changes from COVID19
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
How To Distance Socially without Detaching
“Party of four please!”
I don't know about you, but I’m having a hard time keeping up with the amount of people I can hang out with in the midst of this epidemic. A week ago, the CDC simply recommended canceling large events and mass gatherings for two months, then yesterday the White House instructed America to keep the gatherings to groups of ten or less. Last night our Governor closed all dine-in restaurants and bars at 5pm until further notice.... take out only.
“What’s the goal of all of this distancing?”
The CDC defines social distancing as “remaining out of congregate settings, avoiding mass gatherings, and maintaining distance (approximately 6 feet) from others when possible." The virus seems to be primarily spread through respiratory droplets of an infected person. If you are in close contact with this person (less than six feet for ten minutes or more), there’s a good chance you will contract the virus. The CDC says it may be possible to pick up the coronavirus from countertops and door knobs but that doens’t seem to be the primary vector for transmission… Hence the distancing.
It seems to me that most people think we are going to stay in solitude in our homes until the virus is completely eradicated thereby escaping the contagion completely... not really. Oxford's Our World in Data project explains:
"While the total number who get infected might not change, the containment measures intend to avoid an outbreak trajectory in which a large number of people get sick at the same time."
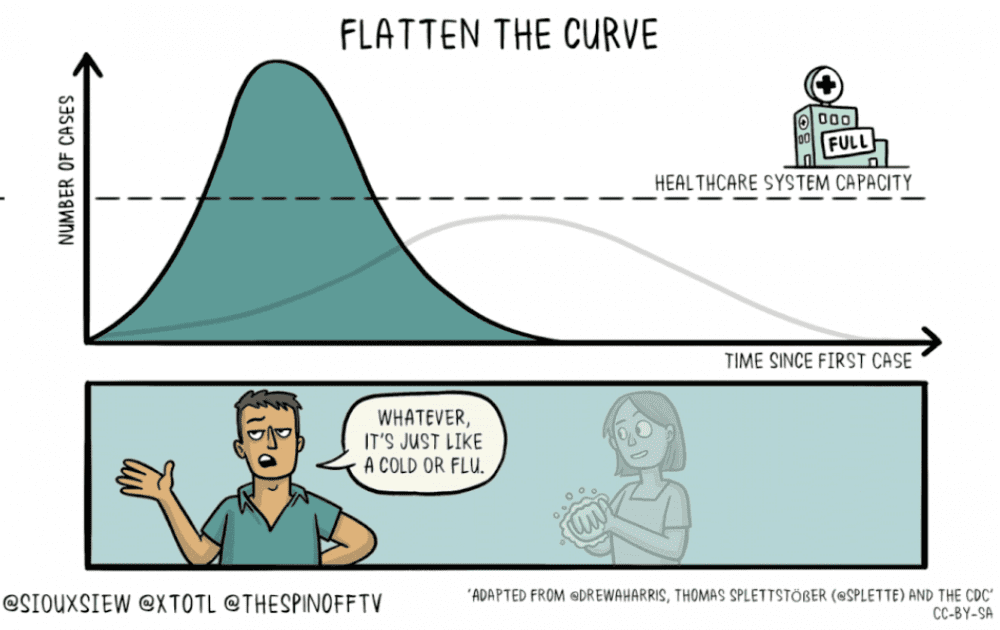
Therefore, staying home and distancing yourself from others is crucial to “flatten the curve” and lesson the number of cases seen daily, weekly and monthly. The goal of this is to reduce the death toll and slow the number of people who contract the virus. This will help our hospitals, medical centers and urgent cares be able to safely take care of those who become ill with the virus as well as those who need medical care for other reasons, like accidents, heart attacks, cancer surgeries, etc.
Many hospitals have tried to prepare by stockpiling extra supplies and training staff in COVID-19 triage procedures. Unfortunately, some hospitals are already showing strain. Vital supplies of personal protective equipment (PPE) are either depleted or set to run out in a matter of days and certain medications made only in China are in short supply. Other hospitals that have been inundated by the virus, like Italy, set the example of what can happen to a hospital system that isn’t prepared for this type of outbreak: not enough ICU rooms, negative pressure rooms or ventilators, and moving critically ill patients out of the ICU so that “sicker” patients can take their place.
“Isn’t this just another flu virus? I’m used to those!”
I hear many people minimizing the situation by saying the coronavirus is just another “flu” and all of this extreme social distancing is off-the-charts insane. I think the gravity of this new virus can be difficult for some to comprehend because we only have our first hand experience to compare it to, and that is our experience with the yearly flu. When people compare the coronavirus to the yearly flu, it normalizes this virus thereby minimizing our concern.
On average, our typical flu season lasts about three months time. Since we can predict the virus type and the season, about 40% of the population receives the flu vaccine prior to the season even starting. The yearly flu season is well-studied and well-prepared for. Epidemiologists can predict where it comes from, when it’s coming and how severe (or not) it will be. Last year 34,200 people died from the flu. In contrast, we don’t know how long this virus will last or even exactly where it came from. We are in the process of studying it while it is causing severe illnesses and deaths. Instead of studying it in a lab, we are studying it on the battlefield.
“What if I need to see my Nurse Practitioner or Doctor?”
If you are mildly ill, the CDC wants you to stay home and call your healthcare provider. If you don’t have a nurse practitioner or doctor, Telemedicine companies like LoginClinics are a great place to start. In fact, the White House and private insurance companies are now covering telemedicine services given this epidemic. LoginClinics’ providers are certified in telemedicine and are able to quickly triage your symptoms and perform a medical evaluation over the internet securely. If everyone with mild respiratory symptoms sought in-person care, it would make the treatment of critically ill patients more difficult. Plus, you would be putting yourself at risk for picking up the virus if you didn’t have it.
The take home message? Stay home if you are mildly ill. Call your nurse practitioner or doctor if you have both a fever and a cough, or use certified telemedicine platforms like LoginClinics. If you develop severe symptoms like shortness of breath, unremitting fever, weakness or lethargy, seek care immediately. Older patients and individuals who have underlying medical conditions or are immunocompromised should contact their nurse practitioner or doctor early in the course of even a mild illness.
If you do not have access to a primary care provider, or don’t have the broadband capacity for a telemedicine visit, contact the Wake County Health Department, or any other North Carolina County Health Department here.
“Can I go to the grocery store?”
Sure, but try to do so not very often. I recommend planning ahead and using grocery store pick up services at Wal-Mart, Target, Lowes or Harris Teeter if you can. These systems are overwhelmed too, so give them a couple of days to prepare your order. Amazon’s Prime Pantry delivers to your home in two days if you are a prime member. There are also other food delivery services like Rastelli’s for meat, Sunbasket, Hello Fresh and Blue Apron . If you can, I recommend shopping local and using Just One More Bite or The Lemon Tree .
“Can I go out to eat?”
No. That would cause a lot of exposure and compromise the group number and distance rule. If you have an urge for chinese food, pizza or sushi, call your favorite restaurant and schedule a curbside pick up, or use delivery services like Uber Eats or Grub Hub.
“What should I avoid until further notice?”
- Gatherings indoors of 5 or more people
- Handshakes and hugs
- Getting close to people who do not reside in your home
- Public places like movie theatres, restaurants, gyms, churches
- Public transportation
- Playdates for your kids
- Nail Salons
- Nursing Homes and Assisted Livings
- Birthday parties, weddings and other celebrations
“What can I do?”
Go outside- spring is upon us! If you see your neighbors, stop and chat with them but reserve the hugs and handshakes for another day. Take your dog or kids for a nature walk. Play tennis, soccer, or basketball in your driveway. My daughter rides horses at an outdoor farm so she has been having fun doing this over her break.
Make a list of things you can do inside your house- you know, that list that you never get to like cleaning the baseboards and reorganizing your closet? Here’s some of the things that are on my list for the next two months:
- Go through clothes and package them up for donation
- Paint my daughter’s room
- Clean and organize my garage
- Organize and clean out my attic
- Daily Unwined on White virtual yoga
- Plant trees outside and mulch the garden beds
- Family game nights
- Read through my book list in double time
- Watch the Seinfeld series from beginning to end, but only 1 per day
- Buy clothing and accessories from Arrow Tree Boutique - delivered for free!
- Quarintine myself in my bedroom with my husband ;)
- Distance learning with the kids
- 20 minutes of reading per day. (Page158 books is providing curbside service!)
- One virtual field trip per day
- Free Scholastic Learning Courses
- Play Alexa Would you Rather or Escape the Room games
- Pen paling
Coordinate with your neighborhood or street to offer a front porch book and game exchange. Our street has a closed facebook group that we use to maintain a sense of community as well as communicate information and needs. I put a bunch of books outside on my porch, took a picture of them and posted them in the group. This way, we have our own internal book and game exchange.
And most of all, don't panic or worry. Find the positives in the social distancing- more time for your spouse, kids and home. More time for things that you've placed on the backburner that just never seen to get taken care of. This too shall pass, but in order for it to pass with the least severe impact on our nation and healthcare system we need to stay distanced, but still stay engaged.
About LoginClinics- Founded by Jaclyn Qualter, a nurse practitioner and health care mentor, in September 2019, LoginClinics provides its fee schedule on its website at www.LoginClinics.com along with FAQs on how to use the online service. More information can be found on its social media www.facebook.com/TelemedicineNC or @loginclinics on Instagram.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor
Coronavirus UPDATE March 15, 2020
Weekly Update
This past week has been like no other I’ve seen in my 20 years in direct patient care. Last year I opened my own telemedicine business- LoginClinics- but didn’t imagine it would be used to screen people virtually for novel coronavirus symptoms. It seems telemedicine is at a tipping point right now as many federal organizations and healthcare institutions are strongly advocating for its use. Only a couple days ago President Trump signed the Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020 (HB 6074) which allows Medicare to reimburse for more TeleHealth services. As a healthcare provider, my email inbox is flooded daily with COVID19 information and position statements from various healthcare companies, medical associations and boards. As a healthcare provider I’m told I need to encourage my patients to stay home and offer telemedicine services delivered via phone, tablet or computer.
COVID-19 Background
Just to recap, the family of coronaviruses have been around for a long time and they are typically responsible for the common cold. The novel, or “new” coronavirus (COVID-19) has produced an epidemic that is similar to the SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome) outbreaks of 2002 and 2015 respectively. Here are are the stats to date:
- SARS: 8,096 cases, 9.6% mortality
- MERS: 2,494 cases, 34% mortality
- COVID-19: 153,524 cases, 3.7% mortality (5,789 deaths)
Let’s Get Scientific… You can do it!
Two recent medical retrospective studies (called this because we can’t select our patient base, we simply look back to gather data) were published on March 11th about COVID19 patients in the Lancet and JAMA. These aren’t medical science gold standard, but it’s the best we have right now.
The Lancet looked at risk factors and the course of COVID19 disease of 191 Wuhan, China patients.
- About half the patients had another medical problem (48%)
- High blood pressure 30%
- Diabetes 19%
- Heart disease 8%
- Increasing age showed a higher risk of death and multi organ failure; kidney failure being the most common
- Contagiousness lasted on average of 20 days, but sometimes lasted up to 37
Since this virus is so new we need to figure out which way to test for it is the best and most accurate. JAMA analyzed over one thousand different lab specimens from 205 patients who were diagnosed with COVID-19. They looked at which types of lab tests would produce the most accurate result (in this case, a positive COVID diagnosis) in someone with the infection. In this study, they found the average age of persons to be 44 with the oldest being 67 and the youngest 5. Almost 70% of the specimens were from men and 19% were described as having “severe illness”. The results showed lung washings to be the most accurate at 68%. The rest were:
- Sputum: 72% accurate
- Nasal swabs: 63% accurate
- Brush biopsy: 46% accurate
- Stool: 29%
- Blood: 1%
- Urine: 0%
Other Scientific Updates
1- Care is supportive. Medications that help slow viral shedding like Tamiflu and Xofluza have not been deemed effective.
2- Trials are underway to test china’s anti-flu drug favilavir , the malaria drug chloroquine, the ebola drug remdesivir, and the HIV drug lopinavir/ritonavir.
CDC Prevention Recommendations Remain Static
- Stay home when you are sick with respiratory disease symptoms. At this time, symptoms are more likely from the flu than COVID-19
- Cover coughs and sneezes with a tissue, then throw it in the trash can
- Wash hands often with soap and water for at least 20 seconds; especially after going to the bathroom, before eating, and after blowing your nose, coughing or sneezing. (If soap and water are not readily available, use an alcohol-based hand sanitizer with 60-95% alcohol.)
- Environmental Health Action: Routinely clean frequently touched surfaces and objects
- Avoid handshakes
- Avoid touching your eyes, nose and mouth
- Cough and sneeze into your elbow, not your hands
- Avoid close contact with anyone who is sick
- Use hand sanitizer between washes
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe
When can I, and how do I get tested?
Currently, tests are in short supply and available on a limited basis. Broader testing may be available and recommended soon through drive though sites hosted at your local Wal-Mart courtesy of the Trump Administration. For now, however, the determination of who to test lies at the sole discretion of the treating medical provider. Priorities for testing may possibly include:
- Any recent travel to a country with a CDC level 2 or Level 3 travel health notice for COVID-19
- Any persons, who within 14 days of symptom onset had close contact with a suspect or laboratory-confirmed4 COVID-19 patient, or who have a history of travel from affected geographic areas within 14 days of their symptom onset.
- Other symptomatic individuals such as, older adults and individuals with chronic medical conditions and/or an immunocompromised state that may put them at higher risk for poor outcomes.
If you’re not sure what kind of symptoms you’re experiencing, or if you don’t have a medical provider, you should use a telemedicine platform like LoginClinics to start. LoginClinics is providing our local community members with $10 Coronavirus Screenings through the end of this month. Simply call, text or schedule an appointment online here.
Steps to take if you feel “flu-ish”:
For the time being, if you feel “flu-ish” you should make the same decisions about seeking medical care as you would normally. Determining whether you have a cold, the flu, bronchitis or pneumonia is important, but this determination needs to be done in the same way as you did before you heard of the COVID epidemic.
Ask yourself this question:
“If I knew nothing about COVID, would I seek medical care right now?”
If your answer is “yes”, then call your doctor. If your answer is “no”, then continue on as you would any other day. We must be careful healthcare consumers right now. We cannot allow ourselves to be motivated by panic and driven by anxiety. We must remain smart and careful and know the resources that are available to us. LoginClinics is here to help with any questions or concerns you may have about your bodily health, your mental health or your risk of having the novel coronavirus. We can guide you and give you recommendations on what to do and how to proceed. If we feel you need to be tested for the virus, we can facilitate that too.
Author: Jaclyn Qualter, Founder, Nurse Practitioner and Healthcare Mentor